Pancreas Diseases
Acute pancreatitis is a serious condition where the pancreas becomes inflamed over a short period of time. Pancreatitis is a disease in which the pancreas becomes swollen and inflamed. During pancreatitis, the digestive enzymes of the pancreas become activated before they are released into the intestine and begin attacking the pancreas itself.
What are the Types of Pancreatitis?
- Acute pancreatitis:Acute pancreatitis is a sudden inflammation of the pancreas. It may range from mild discomfort to a severe, life-threatening illness. Most people with acute pancreatitis recover completely after getting the right treatment. In severe cases, acute pancreatitis can result into: necrosis or death of the pancreatic tissue; bleeding into the gland; infection, and cyst formation. Severe pancreatitis can also harm other vital organs such as the heart, lungs, and kidneys.
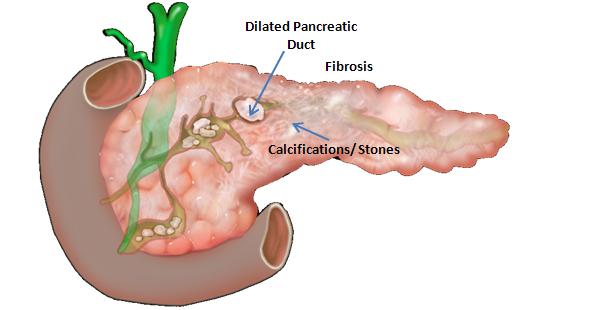
- Chronic pancreatitis:Chronic pancreatitis is long-lasting inflammation of the pancreas. Heavy alcohol drinking is an important cause. Damage to the pancreas from heavy alcohol use may not cause symptoms for many years, but then the person may suddenly develop severe pancreatitis symptoms.
What causes pancreatitis?
- Gallstones
- Heavy alcohol use
- Certain medications
- Infections
- Trauma
- Metabolic disorders
- ERCP
- Surgery
- Unknown cause (idiopathic)
- Long-time alcohol abuse
- Hereditary disorders of the pancreas
- Cystic fibrosis
- High triglycerides
- Tropical pancreatitis
- Unknown cause (idiopathic)
How is pancreatitis diagnosed?
To diagnose acute pancreatitis, doctors measure levels in the blood of two digestive enzymes, amylase and lipase. High levels of these two enzymes strongly suggest acute pancreatitis.
What are the symptoms of acute pancreatitis?
- Upper abdominal pain that radiates into the back; it may be aggravated by eating, especially foods high in fat.
- Swollen and tender abdomen
- Nausea and vomiting
- Fever
- Increased heart rate
How is acute pancreatitis treated?
People with acute pancreatitis are typically treated with IV fluids and pain medications in the hospital. In some patients, the pancreatitis can be severe and they may need to be admitted to an intensive care unit (ICU). In the ICU, the patient is closely watched because pancreatitis can damage the heart, lungs, or kidneys. Some cases of severe pancreatitis can result in death of pancreatic tissue. In these cases, surgery may be necessary to remove the dead or damaged tissue if an infection develops. An acute attack of pancreatitis usually lasts a few days. An acute attack of pancreatitis caused by gallstones may require removal of the gallbladder or surgery of the bile duct. After the gallstones are removed and the inflammation goes away, the pancreas usually returns to normal.
What are the symptoms of chronic pancreatitis?
- Frequently episodes of pain in the upper abdomen that may radiate to the back
- Weight loss
- Diarrhoea
- Steatorrhea (oily stools)
- Backache
- Diabetes mellitus
How is chronic pancreatitis treated?
Chronic pancreatitis can be difficult to treat. Doctors will try to relieve the patient's pain and improve the nutrition problems. Patients are generally given pancreatic enzymes and may need insulin. A low-fat diet may also help. ERCP may be done to place stent in the pancreas and to remove stones. Surgery may be done in some cases to help relieve abdominal pain, restore drainage of pancreatic enzymes or hormones, treat chronic pancreatitis caused by blockage of the pancreatic duct, or reduce the frequency of attacks. Patients must stop smoking and drinking alcoholic beverages, follow their doctor's and dietitian's dietary advice, and take the proper medications in order to have fewer and milder attacks of pancreatitis.